At the Heart of Rural Palliative Medicine
providing palliative medicine training in rural communities.
The Rural and Remote Institute of Palliative Medicine, also known as RRIPM, is a national network of collaborating rural palliative medicine services, working together to support excellent rural training in the specialty area of palliative medicine.
Established in 2023, the Rural and Remote Institute of Palliative Medicine is a program of the Australian and New Zealand Society of Palliative Medicine (ANZSPM).
It is governed by a management committee reporting to the ANZSPM Council with representation from Royal Australasian College of Physicians (RACP) Chapter of Palliative Medicine and other key stakeholder groups.
A sector-wide reference group provides ongoing input to ensure strategic alignment with palliative care developments in the broader health sector.
Find out more about ANZSPM here >>
Around 7 million Australians (28% of the population) live in rural or remote areas (AIHW, 2023).
Only 16% of specialists, however, work in rural areas. As such, there are significant disparities in the kind of palliative care that is available to people in different geographic locations across Australia as they near the end of life.
A national scoping review, completed in March 2023, identified significant opportunities to strengthen rural palliative medicine.
View Beyond the Burbs: Specialist Palliative Medicine Training in Rural Australia – A Scoping Review

The Rural and Remote Institute of Palliative Medicine [RRIPM] is a program supported by ANZSPM with the specific purpose of strengthening access to, and support for, palliative medicine training in rural and remote communities within Australia.
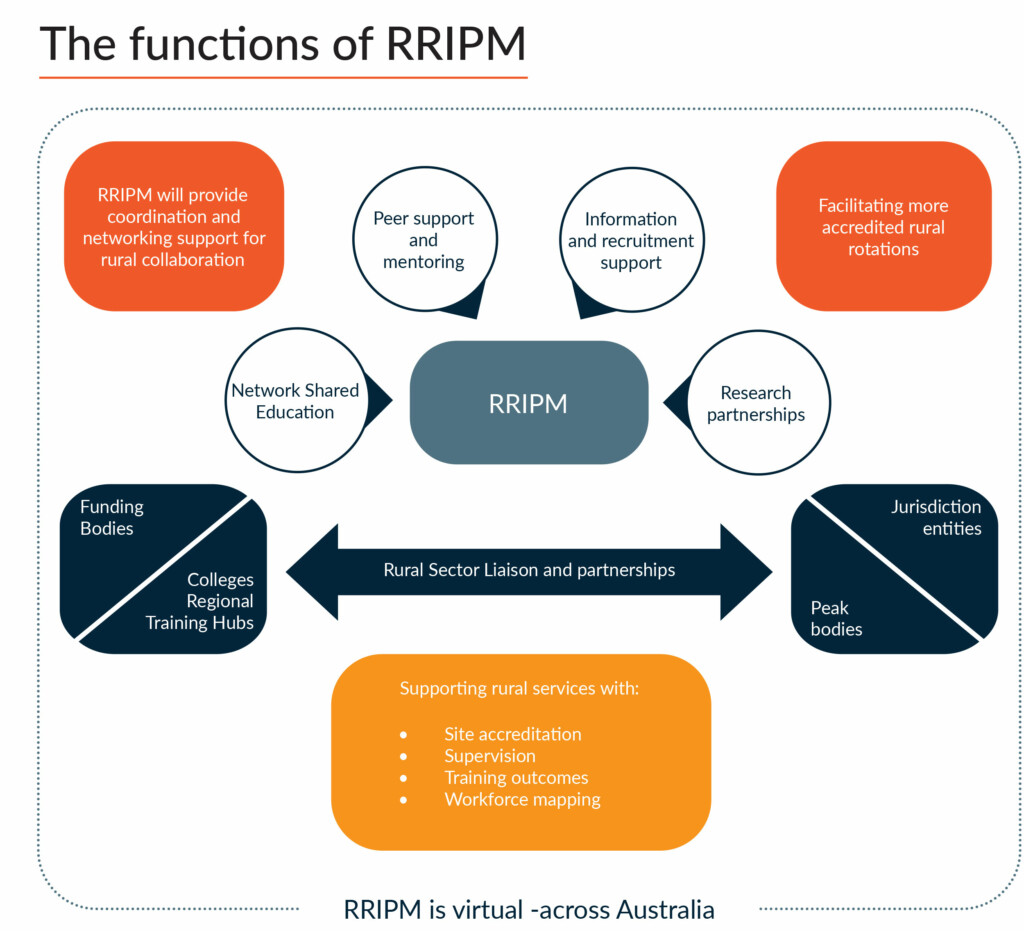
RRIPM will offer an integrated Rural and Remote Training experience:
- designed by rural doctors for rural doctors.
- based on RACP competency-based training curriculum.
- offering a full range of high-quality fully supported rural training experiences.
Our guiding principles
- Our heart is in the country
- Rural training is led by rural services.
- Trainees need access to rural opportunity
- RRIPM fosters, coordinates, and grows the training network so trainees have more choice
- Excellent rural training, focusing on rural competencies, creates excellent clinicians
- Borders are not barriers
- Rural services understand each other
- We can’t dissolve time zones, but we can create latitude in our approach across borders (let’s find a way)
- Our online infrastructure supports trainees and supervisors no matter the time of day
- We’re all in this together
- We care about each other, our collaboration is based on our shared experience, and our systems support us to stay connected.
The Modified Monash Model classifies metropolitan, regional, rural and remote areas according to geographical remoteness, as defined by the Australian Bureau of Statistics (ABS).
The MMM is used to determine eligibility for a range of health workforce programs, such as rural Bulk Billing Incentives, Workforce Incentive Program, Bonded Medical Program.
The RRIPM program has adopted the MMM classification as a guide, operating mostly within areas classified MMM3-7. More information is available here >>


